EVALUATION OF HBA1C IN THE DIAGNOSIS OF DIABETES MELLITUS
Darla Srinivasarao1, Sherafin Jancy Vincy2, Chandrasekar M2
1Division of Medical Lab Technology, School of Medical and Allied Science, Galgotias University, Greater Noida, India
2Sree Balaji College of Physiotherapy, Bharath Institute of Higher Education and Research, Chennai, India.
Research Article
SALT Journal of Scientific Research in Healthcare, Volume 3, Issue 1, Page 17-22, Published on 25th May 2023, https://doi.org/10.56735/saltjsrh.ms2303011722
ABSTRACT
Diabetes mellitus is a prevalent metabolic disorder that requires early detection and effective management. Glycated hemoglobin (HbA1c) evaluation has emerged as a valuable tool in diagnosing diabetes mellitus. This study evaluated 62 cases, with 21 diabetic and 41 non-diabetic, and found a significant p-value for HbA1c levels. The mean HbA1c level was 6.36, with a standard deviation of 1.90 and a variance of 3.6189. Comparative analysis showed an increased case detection rate in HbA1c testing. HbA1c testing improves accuracy and convenience of diabetes diagnosis, correlates with long-term glycemic control, and is a prognostic marker for cardiovascular risk. The study highlights the importance of incorporating HbA1c testing into clinical practice, monitoring treatment effectiveness and guiding therapeutic decisions. The findings support the growing recognition of HbA1c as a reliable diagnostic tool for diabetes mellitus, with its ability to reflect average blood glucose levels over a prolonged period. Further research is needed to explore its applicability across different populations and establish standardized guidelines for HbA1c interpretation and utilization.
Keywords: Diabetes mellitus, HbA1c, Diagnostic tool, Glycemic control, Fasting, Post prandial
INTRODUCTION
Diabetes mellitus is a prevalent metabolic disorder characterized by chronic hyperglycemia caused by insulin deficiency, insulin resistance, or a combination of both1. It is a major global health concern, with an estimated 463 million adults affected worldwide in 2019, and is projected to rise to 700 million by 2045. Diagnosis of diabetes is crucial for timely intervention and appropriate management to prevent or delay complications. The National Academy of Clinical Biochemistry (NACB) issued its “Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus” in 2002 2.
Traditionally, diagnostic tests like fasting and postprandial blood glucose assessments have been used for diagnosing diabetes, but they may not accurately capture long-term glycemic control. In recent years, the evaluation of glycated hemoglobin (HbA1c) has emerged as a valuable and widely accepted tool for diagnosing diabetes mellitus. HbA1c is a form of hemoglobin that reflects the average blood glucose concentration over a period of approximately two to three months. It forms through a non-enzymatic process called glycation, where glucose molecules bind to hemoglobin in red blood cells 3.
The American Diabetes Association (ADA)4, World Health Organization (WHO), and other prominent diabetes organizations recognize the importance of HbA1c as a diagnostic tool. The ADA recommends using HbA1c levels of 6.5% (48 mmol/mol) or higher as a diagnostic criterion for diabetes. This approach offers several advantages over traditional glucose-based tests, such as convenience, reliability, and integration of long-term glucose data5.
The objective of the present study is to explore the efficacy and significance of HbA1c in the diagnosis of diabetes mellitus, focusing on its advantages over other diagnostic methods like fasting and postprandial glucose tests. The potential implications of incorporating HbA1c testing into clinical practice include early detection, improved disease management, and prevention of complications associated with diabetes.
MATERIALS AND METHODS
Study Design
The study evaluated HbA1c’s efficacy in diagnosing diabetes mellitus using a cross-sectional design, involving participants at Chennai.
Participants
The study enrolled 62 individuals aged 25-75, with 40 males and 22 females, obtaining informed consent before inclusion.
Diagnostic Tests
The diagnostic tests conducted in this study included fasting and postprandial blood glucose assessments, as well as the measurement of HbA1c levels. The fasting blood glucose test was performed after an overnight fast, typically for a minimum of 8 hours. The postprandial test involved measuring blood glucose levels two hours after a standardized meal. Both tests were carried out using standard protocols and equipment6. HbA1c levels were measured using a standardized laboratory assay, determining the percentage of HbA1c in total hemoglobin. This indicates the average blood glucose concentration over the past two to three months 7.
Data Collection
Demographic data, including age and gender distribution, was collected for analysis. Participants were categorized into age groups, with male and female participants analyzed to determine diabetes prevalence variations. Recorded participants fasting and postprandial blood glucose tests, along with HbA1c levels, to compare HbA1c diagnostic efficacy against traditional glucose-based tests.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software. Descriptive statistics were employed to summarize the data, including means, standard deviations, and variances. The significance of the results was assessed using inferential statistics. A p-value of less than 0.005 was considered statistically significant for this study. The association between HbA1c levels and the diagnosis of diabetes was evaluated using appropriate statistical tests, such as chi-square analysis or t-tests, depending on the nature of the data.
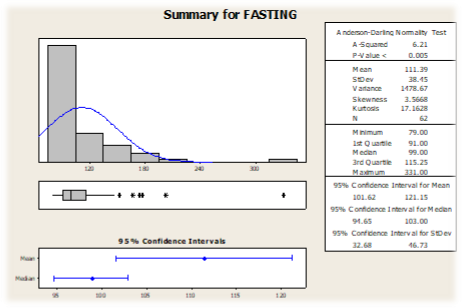
Graph 1 Shows the summary for fasting blood sugar
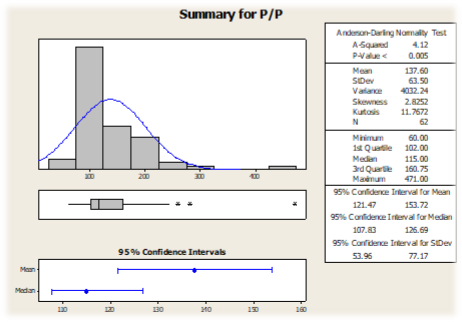
Graph 2 Shows the summary for post prandial blood sugar
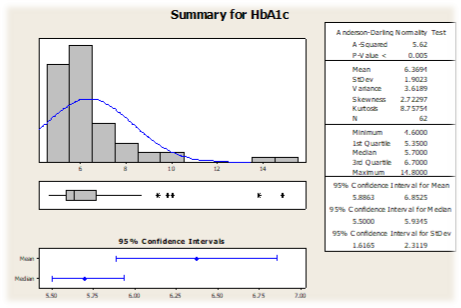
Graph 3 Shows the summary for HbA1C
Ethical Considerations
The study adhered to ethical guidelines, obtained informed consent from participants, and ensured privacy and confidentiality. The research protocol
RESULTS
Demographic Characteristics
The study included a total of 62 participants, comprising 40 males and 22 females. The age range of the participants varied from 25 to 75 years. The distribution of participants across different age groups was as follows: 8 males and 5 females in the age group of 25 to 35, 11 males and 4 females in the age group of 36 to 45, 5 males and 6 females in the age group of 46 to 55, 9 males and 4 females in the age group of 56 to 65, and 7 males and 3 females in the age group of 66 to 75.
Diabetic Cases
Among the 62 participants, 21 were diagnosed with diabetes based on the diagnostic criteria used in this study. Out of these 21 diabetic cases, 13 were male and 8 were female. The remaining 41 participants were classified as non-diabetic, with 27 males and 14 females in this group.
Fasting Blood Glucose
Among the 21 diabetic cases, fasting blood glucose levels above the diagnostic threshold were observed in all individuals. In the non-diabetic group, 27 participants had fasting blood glucose levels within the normal range, while 14 participants had elevated fasting blood glucose levels (Graph 1).
Postprandial Blood Glucose
Similar to the fasting blood glucose results, all 21 diabetic cases exhibited postprandial blood glucose levels exceeding the diagnostic cutoff. In the non-diabetic group, 27 participants had postprandial blood glucose levels within the normal range, while 14 participants had elevated postprandial blood glucose levels (Graph 2).
HbA1c Levels
Evaluation of HbA1c levels revealed that among the 21 diabetic cases, 13 males and 8 females had HbA1c levels indicating diabetes. In the non-diabetic group, 27 males and 14 females had HbA1c levels within the normal range (Graph 3).
Statistical Analysis
The statistical analysis, performed using SPSS software, indicated a significant association between HbA1c levels and the diagnosis of diabetes. The obtained p-value (p<0.005) suggested a strong relationship between HbA1c levels and diabetes diagnosis. The mean HbA1c level in the study population was found to be 6.36, with a standard deviation of 1.90. The variance of HbA1c levels was calculated to be 3.6189.
Case Detection Rate
Comparing the case detection rates of fasting and postprandial blood glucose tests with HbA1c, it was observed that HbA1c detected a higher number of diabetic cases. Among the 62 participants, the fasting and postprandial tests identified 21 individuals with diabetes, whereas HbA1c identified 24 individuals with diabetes. This finding indicates that the case detection rate increased when HbA1c testing was incorporated into the diagnostic protocol.
Overall the study shows that HbA1c is an effective diagnostic tool for diabetes mellitus, with significant associations with diagnosis. HbA1c levels provide insight into glycemic control and have a higher case detection rate, emphasizing its importance in identifying individuals with diabetes, enabling early intervention and improved disease management.
DISCUSSION
The evaluation of HbA1c in the diagnosis of diabetes mellitus has gained significant attention in recent years due to its potential advantages over traditional glucose-based tests. In this study, we aimed to explore the efficacy and significance of HbA1c as a diagnostic tool for diabetes, compare it with fasting and postprandial blood glucose tests, and discuss its potential implications for clinical practice 8.
The results of our study demonstrated a significant association between HbA1c levels and the diagnosis of diabetes. All 21 individuals diagnosed with diabetes exhibited elevated HbA1c levels, indicating a strong correlation between HbA1c and the presence of diabetes. This finding aligns with the diagnostic criteria recommended by major diabetes organizations, such as the ADA and WHO, which consider HbA1c levels of 6.5% (48 mmol/mol) or higher as indicative of diabetes. Our study supports the use of HbA1c as a reliable diagnostic marker for diabetes mellitus.
One of the key advantages of HbA1c testing is its convenience. Unlike fasting and postprandial blood glucose tests, HbA1c measurement does not require specific timing or patient preparation. Patients can undergo HbA1c testing at any time of the day, regardless of their recent food intake. This convenience enhances patient compliance and reduces logistical challenges associated with traditional glucose tests, making HbA1c a more practical and accessible diagnostic tool. Furthermore, HbA1c provides an integrated assessment of long-term glycemic control, reflecting average blood glucose levels over a period of two to three months. It eliminates the inherent variability associated with fasting and postprandial glucose tests, which are influenced by short-term fluctuations due to factors such as recent meals, stress, or illness. HbA1c, being less affected by these factors, offers a more stable and reliable indicator of overall glycemic control. This stability makes HbA1c a valuable tool not only for diagnosing diabetes but also for monitoring treatment efficacy and long-term disease management 9.
In our study, the case detection rate increased when HbA1c testing was incorporated into the diagnostic protocol. HbA1c identified three additional diabetic cases compared to fasting and postprandial glucose tests alone. This finding highlights the superior sensitivity of HbA1c in detecting individuals with diabetes, further emphasizing its significance in early detection and intervention. Identifying diabetes cases promptly allows for timely initiation of treatment, leading to better glycemic control and a reduced risk of complications associated with diabetes 10.
LIMITATIONS
This study has limitations, including a small sample size, a specific laboratory setting, potential selection bias, and a cross-sectional design. However, it contributes to the existing knowledge on HbA1c diagnostic efficacy in diabetes mellitus and offers valuable insights into its potential clinical benefits. The study’s cross-sectional design provides a snapshot of participants’ glycemic status at assessment time 11.
CONCLUSION
HbA1c evaluation in diabetes diagnosis offers advantages over traditional glucose-based tests, providing a convenient, stable, and integrated assessment of glycemic control. The strong association between HbA1c levels and diabetes diagnosis supports its inclusion in routine clinical practice. Early detection and intervention contribute to improved patient outcomes and effective management of diabetes mellitus. Further research and integration into diagnostic protocols will enhance the understanding and utilization of HBA1c in diabetes care.
REFERENCES
- Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997 Jul; 20(7): 1183-97. https://doi.org/10.2337/diacare.20.7.1183. PMID: 9203460.
- Sacks DB, Bruns DE, Goldstein DE, Maclaren NK, McDonald JM, Parrott M. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem. 2002; 48: 436–72.
- Nathan DM, Singer DE, Hurxthal K, Goodson JD. The clinical information value of the glycosylated hemoglobin assay. N Engl J Med. 1984 Feb 9; 310(6): 341-6. https://doi.org/10.1056/NEJM198402093100602. PMID: 6690962.
- Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan D, Peterson CM, Sacks DB. Tests of glycemia in diabetes. Diabetes Care. 2004 Jul; 27(7): 1761-73. https://doi.org/10.2337/diacare.27.7.1761. PMID: 15220264.
- Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE; NGSP Steering Committee. The national glycohemoglobin standardization program: a five-year progress report. Clin Chem. 2001 Nov; 47(11): 1985-92. PMID: 11673367.
- Ketema EB, Kibret KT. Correlation of fasting and postprandial plasma glucose with HbA1c in assessing glycemic control; systematic review and meta-analysis. Arch Public Health. 2015 Sep 25; 73: 43. https://doi.org/10.1186/s13690-015-0088-6. PMID: 26413295; PMCID: PMC4582842.
- Saudek CD, Derr RL, Kalyani RR. Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA. 2006 Apr 12; 295(14): 1688-97. https://doi.org/10.1001/jama.295.14.1688. PMID: 16609091.
- Florkowski C. HbA1c as a Diagnostic Test for Diabetes Mellitus – Reviewing the Evidence. Clin Biochem Rev. 2013 Aug; 34(2):75-83. PMID: 24151343; PMCID: PMC3799221.
- Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomark Insights. 2016 Jul 3; 11: 95-104. https://doi.org/10.4137/BMI.S38440. PMID: 27398023; PMCID: PMC4933534.
- Nathan DM, Balkau B, Bonora E, Borch-Johnsen K, Buse JB, Colagiuri S, et al. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care [Internet]. 2009; 32: 1327–34. https://doi.org/10.2337/dc09-9033.
- Faber J, Fonseca LM. How sample size influences research outcomes. Dental Press J Orthod. 2014 Jul-Aug;19(4):27-9. https://doi.org/ 10.1590/2176-9451.19.4.027-029.ebo. PMID: 25279518; PMCID: PMC4296634.
ARTICLE TYPE: Review Article; ORCID ID: Open Researcher and Contributor Identifier (ORCID) ID of corresponding author: https://orcid.org/0000-0002-7366-2529 ; ETHICAL: Institutional ethical committee and prior patient consent obtained; ACKNOWLEDGEMENT: None; FINANCIAL DISCLOSURE: The authors declare that there was no financial aid received.; CONFLICT OF INTEREST: No conflict of interest associated with this research work.; AUTHORS CONTRIBUTION: D.S., Investigation; M.C., Conceptualisation and methodology; S.J.V., Result analysis and writing; AUTHORS AFFILIATIONS: Mr. Darla Srinivasarao, Assistant Professor, Department of Medical Lab Technology, School of Medical and Allied Science, Galgotias University, Greater Noida, India.; Dr. Sherafin Jancy Vincy, Professor, Sree Balaji College of Physiotherapy, Bharath Institute of Higher Education and Research, Chennai, India. Dr. M Chandrasekar, Professor, Sree Balaji College of Physiotherapy, Bharath Institute of Higher Education and Research, Chennai, India.; CORRESPONDING AUTHOR EMAIL: [email protected]; ARTICLE CITATION: Darla Srinivasarao, Sherafin Jancy Vincy, Chandrasekar M. A evaluation of HbA1C in the diagnosis of diabetes mellitus. SALT J Sci Res Healthc. 2023 May 25; 3(1): 17-22.
PUBLISHER’S NOTE: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
© Darla Srinivasarao, Sherafin Jancy Vincy, Chandrasekar M
Originally published in the SALT Journal of Scientific Research in Healthcare (https://saltjsrh.in/), 25.05.2023.
This is an open-access article distributed under the terms of the Creative Commons License (https://creativecommons.org/licenses/by-nc-nd/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the SALT Journal of Scientific Research in Healthcare (https://saltjsrh.in/), is properly cited. The complete bibliographic information, a link to the original publication on https://saltjsrh.in/, as well as this copyright and license information must be included.